[vc_row][vc_column width="1/1"][vc_column_text]By: Dr. Corey Finan DC
What exactly is Sciatica?
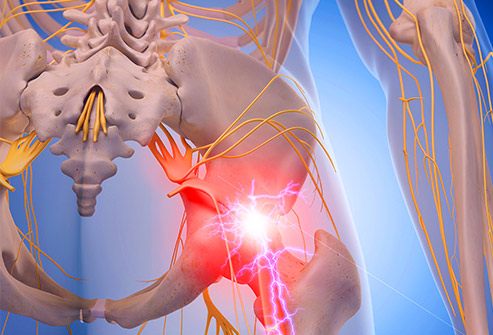
Well, besides being a scary sounding problem, it is one of the most misunderstood health care conditions out there. Why is that? Well, to begin with, true sciatica is a very narrowly defined condition. Wikipedia, and the Merriam-Webster Dictionary all define it as “pain along the course of a sciatic nerve especially in the back of the thigh broadly : pain in the lower back, buttocks, hips, or adjacent parts”. The Mayo Clinic, WebMD and Merck Manual go further and describe how it originates “Sciatica most commonly occurs when a herniated disk, bone spur on the spine or narrowing of the spine (spinal stenosis) compresses part of the nerve.” The resulting symptoms are usually pain, and often numbness in the affected leg. Typically the pain will radiate down the back of the leg past the knee to the foot. When the nerve is compressed (i.e. pinched) you will typically get numbness in the leg from the point of compression down. This numbness is the result of the nerve signal not being able to get from the area downstream of the compression up to the brain which is upstream of the compression. Thus the brain gets no signal from the downstream part of the leg, and our brain interprets a lack of signal into what we call numbness.
We’ve established that most true Sciatica comes from nerve compression in the low back either due to a disc issue, spinal stenosis (closing of the opening for the spinal cord due to increased bone growth), or bone spurs that affect the nerve roots in the back. None of these sound like fun, nor do they sound like things that just happen. In fact other than the disc derangements that can cause sciatica, none of the conditions that cause sciatica are quick. There is usually some indication that things are going gravely wrong in your back long before you get Sciatica.
Just to clarify, what we know about true sciatica is that it is often slow developing (over years), is usually due to some form of alteration in the structures of the low back, and often will have numbness and radiating leg pain as symptoms. Other indications can lead to the diagnosis of true sciatica, such as clinically having a positive Straight Leg Raise, Well Leg Raise, and / or Slump test. Each of these orthopedic tests look at how the spinal nerves are moving within the spinal cord, and if there is an issue such as any of the items that can cause sciatica, you will get a painful positive result on the tests.
Why do I keep saying “true” when referring to Sciatica? For the simple reason that people get leg pain, but it is not due to any of the conditions outlined above. So a new designation was coined for all other causes of Sciatica, and those terms are “False Sciatica”, “Pseudo-Sciatica”, “Sciatica-Like pain syndrome”, and the list goes on and on.
Why is it important to distinguish between true sciatica and all others? Because statistics show that of those with true sciatica, 90% are caused by either disc derangements, bone spurs, and stenosis in the spine. The other 10% are caused by varying conditions including space occupying lesions (tumors), neurodegenerative conditions, and more obscure conditions. So then if 90% of true sciatica is due to low back irregularities, what percentage of people coming in with leg pain is made up of people with true sciatica? According to a 2007 study published in the British Medical Journal, about 5-10% of people with low back and/or leg pain have true sciatica. So, when you crunch the numbers, you have 90% of 10%, or 9% of the total number of people coming in with low back and leg pain being due to true sciatica. To put it into context, in my busy practise over the course of a complete year I may see between 5 and 20 patients that have True Sciatica, while I see upwards of 100’s that have Pseudo Sciatica.
Why is this important? Because there is a saying that goes like this: “If you live in Alberta and you hear the sound of hooves behind you, you should think ‘A horse is coming’”. And if you lived in Africa, you’d think “A Zebra is coming”. The point is, you should look for the most common cause to be the most likely cause, unless something points you in another direction.
So, we have established that most radiating leg pain that comes into a common practise will MOST LIKELY be from something other than a spinal condition that pinches the sciatic nerve. What does that leave us with as the most common cause of radiating leg pain? It may surprise you to find out that it is actually trigger points in the muscles in and around the hip. Most hip muscles will refer pain down the leg in a rather predictable pattern. Trigger points arise in muscles due to overuse. They are focal points within a muscle that maintain a spontaneous electrical activity when at rest while the rest of the muscle exhibits no resting electrical activity. Most people call them “Muscle Knots”, because you can feel them as tightened bands within the muscle belly. It is not surprising that the mother of trigger point research Dr. Janet Travell, M.D. called the Gluteus Minimus the pseudo-sciatic muscle, because even back in the 1970’s when she was doing her research she realized that trigger points within that muscle mimicked the pain that true sciatica caused patients. The only difference is that the Gluteus Minimus is much more common a cause of leg pain that true sciatica.
Another very common cause of referred leg pain can be from sciatic nerve irritation as it exits the hip through the piriformis muscle before darting down the leg. Inflammation can irritate nerves, and an inflamed piriformis can trigger leg pain that runs down the back of your leg. This is common enough to have a syndrome named after it, appropriately called Piriformis Syndrome.
These two muscle conditions are the most common causes of leg pain that goes down the back or side of the leg ending either above or below the knee. They typically are seen in patients who sit for long periods at work, engage in strenuous activities involving the hips (jumping sports, running sports, dancing, etc.), and people who are unable to properly engage their core prior to leg movement. These all set up the environment for the hip muscles to become overused, tired, and tight. This process develops slowly over a number of weeks or years. Once the muscles reach a certain point they become so tight that trigger points can develop.
The good news is hip muscle strains / trigger points are fixable. Active Release Technique (a chiropractic soft tissue treatment involving stretching and releasing of trigger points, fascial restriction, and muscle tightness) can effectively reduce the trigger points and resolve your leg pain. Further, dry needling into the trigger point can be of benefit for stubborn cases. By releasing the tension within the hip muscles, the pain will dissipate, and functionally normal range of motion can be re-established, leading to proper joint function, and feeling better. At Active Sports Therapy we can effectively treat your leg pain and get you back to doing what you love best.
*This blog is not intended to officially establish a physician-patient relationship, to replace the services of a trained physician, naturopathic doctor, physical therapist or chiropractor or otherwise to be a substitute for professional medical advice, diagnosis, or treatment. [/vc_column_text][/vc_column][/vc_row]